-
+1 700 888 1234
-
Effingerstrasse 40 3008 Bern Switzerland
To reach the diagnosis of lung cancer and know the spread of the tumour, a series of tests will be necessary: medical history, physical exam, blood tests, computed tomography (CT) of the chest and upper abdomen, and biopsy.
In some cases, treatment for smoking or additional tests can be necessary, for example, other imaging, lung functioning or biomarker tests.

The first thing the doctor does is to investigate the patient’s history or medical record. This includes questions to the patient about his/her health problems and treatments received during their life. Other questions are about the patient’s symptoms, and about medicines that the patient is taking now or has previously taken.
Doctors ask about symptoms that may be related to lung cancer, such as: cough, chest pain, difficulty in breathing, loss of weight and appetite , etc. To know these details is very important for doctors when staging the lung cancer.
Doctors also ask about the medical history of close blood relatives of the patient, because some cancers may exist in families. The members of the patient’s family who are important for medical history are parents, grandparents and siblings. And the age at which a relative had the disease is also important.
Doctors also ask about smoking: whether the patient smokes or has smoked in the past. The total amount smoked is calculated by packets per day and number of years of smoking.

This is the study of the patient’s body, and its purpose is to look for signs of the disease. For example, in the examination the doctor hears the noise that the air makes when it goes in and out of the lungs. If there is an abnormal noise, this may be a sign of lung disease.
The physical exam includes the measurement of the temperature and weight of the body and the measurement of the pulse, blood pressure, and breathing rate. Doctors listen to the patient’s lungs, heart and gut, and also examine the nose, ears, mouth, eyes and skin. Another assessment is of performance: the patient’s ability to do daily activities, which is useful for knowing whether the patient can undergo certain treatments or not.
The basic laboratory tests give a picture of the patient’s general health. They are usually: 1) Complete blood count (CBC), which measures parts of the blood, including red blood cells, white blood cells and platelets. The number of these cells can change in cancer and other diseases, and some treatments can also cause changes. 2) Biochemistry profile, which serves to know how the kidneys, liver, bone and other organs are working. Abnormal biochemical levels can be caused by the spread of cancer or by other health problems.
There are other laboratory tests for testing biomarkers, usually on tissue samples. Biomarkers are molecules which can be in the tumour, and their presence or absence is used to plan treatment, since some treatments are only effective in tumours with a certain biomarker. Examples of biomarkers are mutations in the EGFR gene or rearrangements in the ALK gene.

Imaging refers to pictures of the inside of the body. It serves to see which parts of the body have cancer. It is performed and interpreted by radiologists. Some imaging uses contrast. This is a ‘dye’ that makes the picture clearer.
Sometimes a lung nodule is found by chance with imaging, and at other times when evaluating a patient with symptoms compatible with lung cancer. The tumour is visible in imaging: a computed tomography (CT) or a positron emission tomography (PET). When CT and PET are used together it is called a PET/CT scan. The characteristics of the lung nodule allow radiologists to know whether it can be a lung cancer. For example, large nodules are more likely to be cancerous than small nodules. And the density of the nodule is important because it is usually related to the speed of growth of the tumour.
Imaging of the chest and upper abdomen serves to find the tumour and to know where to perform the biopsy, and also for identifying the stage of the cancer.
Additionally, there are some imaging tests to check whether there is metastasis of cancer outside the lung: 1) FDG PET/CT is performed with a radiotracer called fluorodeoxyglucose (FDG). This is a radioactive marker that accumulates at the points where cancer cells exist, and they can be seen with this technique. 2) Magnetic resonance imaging (MRI).

Figure. Computed tomography (CT) machine. 
Figure. PET/CT machine. To confirm the existence and know the type of lung cancer it is necessary to see the cells of the tumour by microscopy. These cells can be obtained by: 1) removing tissue samples, which is a biopsy, or 2) removing fluid samples, or aspirating cells with a needle, which is a cytology, because the sample is composed of cells more than tissue.
Histopathological tests will be performed on the tumour and lymph nodes removed by surgery. And before this, in some cases there will be a biopsy using bronchoscopy, a procedure to see the inside of airways and take some samples. To analyse lymph nodes there is a procedure called mediastinoscopy, which allows surgeons to see and perform biopsy on lymph nodes between lungs, and the results of their histopathological tests are useful for staging lung cancer. Sometimes staging can be done with mediastinoscopy without bronchoscopy. And sometimes biopsy might not be done until the surgeon proceeds to remove the tumour.
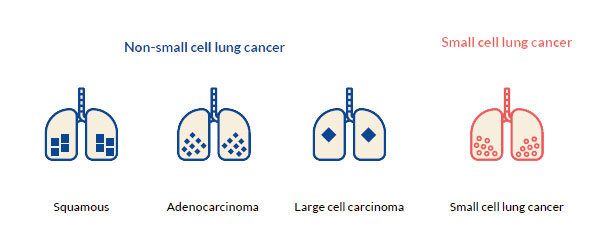
Lung carcinomas are divided into two groups based on how the cancer cells look by microscopy. This is called histologic typing:4,7
There are more types of NSCLC which are rare, for example, the adenosquamous carcinoma, the sarcomatoid carcinoma, etc.